Submitting Claims for Mifegymiso
This topic is intended for Independent pharmacies only and is not applicable to Rexall pharmacies.
Select the applicable tab to learn about submitting claims for Mifegymiso in your province.
Mifegymiso (mifepristone and misoprostol) is covered under PharmaCare for British Columbia residents with a valid prescription.
To bill Mifegymiso to PharmaCare:
-
Create a new prescription for the patient.
-
DIN = 2444038
-
QA and Qty = 5
A TP Rule has been added in the Drug Folder to submit a quantity of 1 to Pharmacare.
-
-
In Rx Detail, ensure the prescription's Bill Code is PC/CA.
-
Ensure all amounts in the Price section are $0.00. If not, perform the following steps:
-
Select the expander button
 to open the Requested Cost window.
to open the Requested Cost window. -
Select the Price Override checkbox.
-
Update the cost, fee, and/or markup to $0.
-
Select OK once done.
-
-
Select Fill.
Patient Eligibility
Mifegymiso (mifepristone and misoprostol) is publicly funded for both ODB and non-ODB recipients. Select the dropdowns below to learn more about the billing information required for each type of patient.
To bill a publicly funded fee for service claim for an ODB-eligible patient, the following Third Party information must be added to the patient’s Third Party tab:
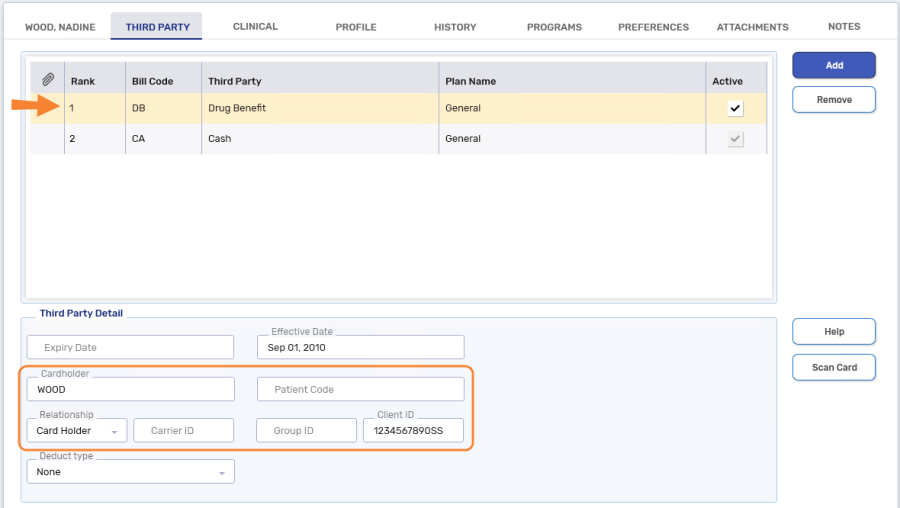
-
Bill Code = DB (Drug Benefit)
-
Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Client ID = patient's health card number
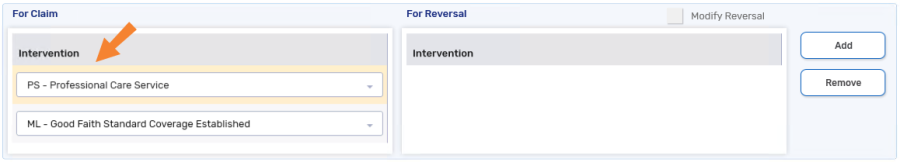
When billing the claim, the following intervention code is required in the Rx Detail > Third Party tab:
-
PS - Professional Care Service

To bill a publicly funded fee for service claim for a non-ODB recipient with a valid Ontario health card number, the following Third Party information must be added to the patient’s Third Party tab:
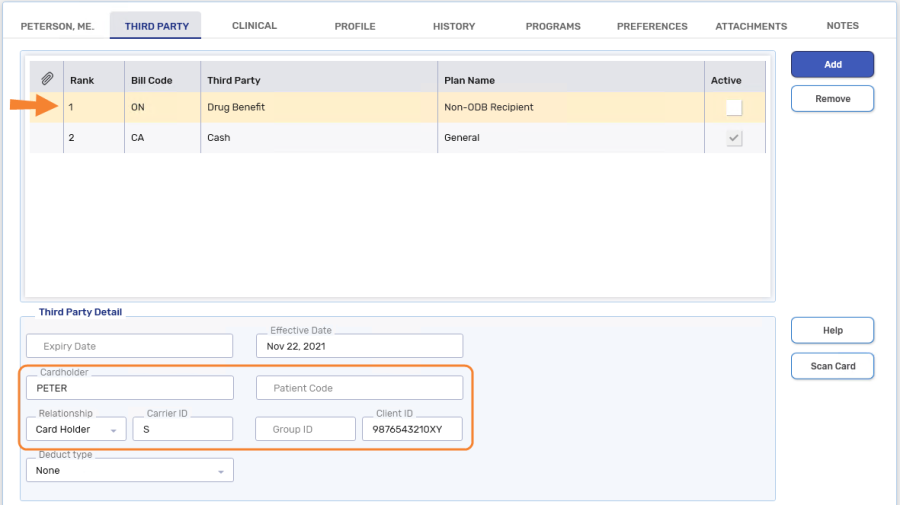
-
Bill Code = ON (Drug Benefit - Non-ODB Recipient)
- Cardholder = The first 5 characters of the patient's last name (entering the patient's complete last name is also acceptable)
-
Relationship = Card Holder
-
Carrier ID = S
-
Client ID = patient's health card number
As with all claims submitted to ODB, the patient’s gender and birth date must be recorded in the Patient Folder.
When billing the claim, the following intervention codes are required in the Rx Detail > Third Party tab:
-
PS - Professional Care Service
-
ML - Good Faith Standard Coverage
Setting Up the Pricing Strategy
By setting up a Pricing Strategy, the correct cost, markup, and fee auto-populate when billing a Mifegymiso prescription to ODB.
To set up the Mifegymiso Pricing Strategy:
-
Open the Drug Folder.
-
Select the Alternative tab.
-
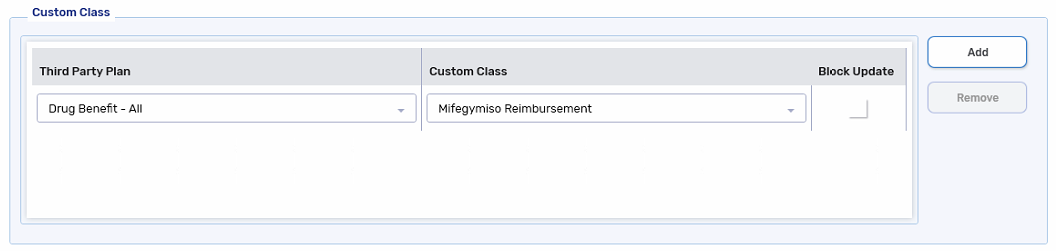
In the Custom Class section, confirm the Custom Class, Mifegymiso Reimbursement is entered for Drug Benefit - All. If not, select Add to add it. Select Save once done.
-
Select More > Pricing.
-
Highlight the Drug Benefit row and select Add. The Create New Strategy window opens.
-
Dropdown the Custom Class field and select Mifegymiso Reimbursement.
-
Select OK.
-
In the Fixed Rules section, set the following fields:
-
Fee = $337.25
-
Markup% = 0%
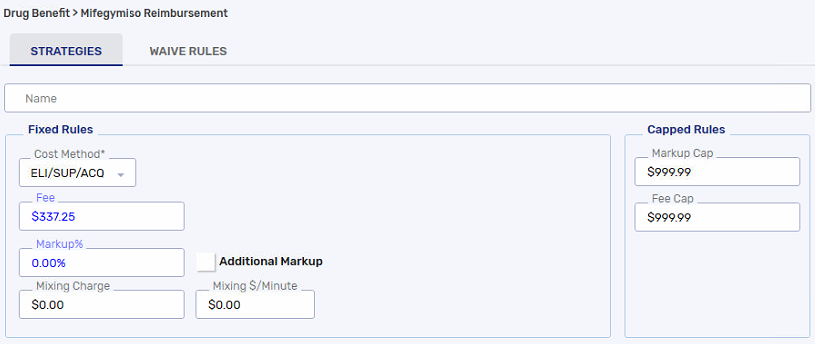
-
-
In the Variable Rules section, select Add. The Add Variable Rule window opens.
-
Set up the window as follows:
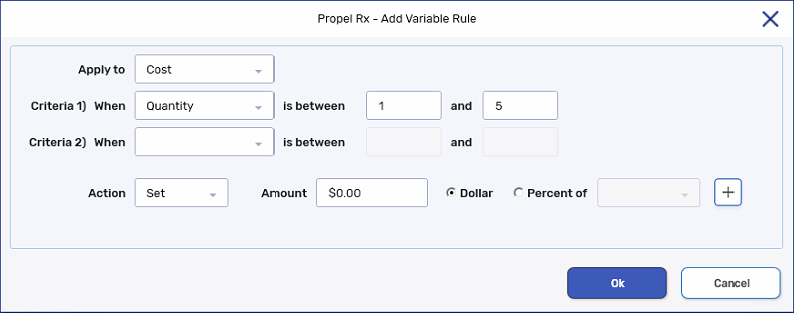
-
Select OK.
-
Select Save.
Billing Mifegymiso for ODB Eligible Recipients (DB/TR)
To bill Mifegymiso for patients covered under ODB:
-
Create a new prescription for the patient for DIN 2444038.
-
In Rx Detail, confirm the following:
-
Cost and Markup = $0.00
- Dispensing Fee = $337.25
-
-
Select the Third Party tab in Rx Detail.
-
Select Add to add PS - Professional Care Service if it is not already entered.
-
Select Fill.
Billing Mifegymiso for Non-ODB Eligible Recipients
To bill Mifegymiso for patients not covered under ODB:
- Create a new prescription for the patient for DIN 2444038.
-
In Rx Detail, confirm the following:
-
Cost and Markup = $0.00
- Dispensing Fee = $337.25
-
-
Select the Third Party tab in Rx Detail.
-
Select Add to add PS - Professional Care Service and ML - Good Faith Standard Coverage if they are not already entered.
-
Select Fill.